Healthcare is a fundamental right, yet for many LGBTQ individuals, accessing equitable medical care remains a significant challenge. According to a recent survey, 1 in 3 LGBTQ adults report experiencing discrimination from healthcare providers. This discrimination can manifest in various ways, from outright refusal of care to subtle biases that impact the quality of treatment received.
The Problem
A study by the Center for American Progress highlights the prevalence of discrimination in healthcare settings. The report found that 29% of LGBTQ adults and 56% of transgender individuals have faced discrimination from healthcare providers. These experiences range from being verbally harassed or refused care outright to having a provider refuse to touch them or use excessive precautions .
Impact on Health Outcomes
Discriminatory practices in healthcare contribute to negative health outcomes for LGBTQ individuals. Fear of discrimination can lead to delays in seeking care or avoidance of healthcare altogether. This avoidance can exacerbate health issues, making them more severe and harder to treat when care is finally sought.
A 2020 report by the National Academies of Sciences, Engineering, and Medicine underscores the importance of culturally competent care. It notes that LGBTQ individuals who experience discrimination in healthcare are more likely to suffer from chronic conditions, mental health issues, and overall poorer health outcomes compared to their heterosexual and cisgender counterparts .
The Role of Implicit Bias
Implicit bias among healthcare providers plays a significant role in the treatment disparities faced by LGBTQ individuals. These biases are often unconscious but can influence clinical decisions, resulting in differential treatment. For example, LGBTQ patients may receive fewer pain medications than their heterosexual counterparts or might be unfairly judged for their lifestyle choices, leading to inadequate care .
Steps Toward Improvement
Addressing these disparities requires a multifaceted approach:
- Education and Training: Healthcare providers must receive comprehensive training on LGBTQ health issues and the unique challenges faced by this community. This training should include cultural competency, understanding implicit biases, and learning best practices for providing equitable care.
- Policy Changes: Implementing non-discrimination policies at both the institutional and governmental levels can provide protections for LGBTQ individuals. The Affordable Care Act’s Section 1557, which prohibits discrimination based on sex, including gender identity, is a crucial step in this direction .
- Patient Advocacy: Encouraging LGBTQ individuals to advocate for themselves and report instances of discrimination can help to highlight the issue and push for systemic changes. Organizations such as Lambda Legal and the Human Rights Campaign provide resources and support for those facing discrimination .
- Research and Data Collection: Collecting data on LGBTQ health outcomes and experiences can help to identify disparities and monitor progress over time. This data is essential for developing targeted interventions and policies to improve healthcare equity.
The statistic that 1 in 3 LGBTQ adults face discrimination from healthcare providers is a stark reminder of the work that remains to be done to achieve healthcare equity. By addressing implicit biases, implementing robust non-discrimination policies, and fostering an inclusive environment, the healthcare system can move towards providing equitable care for all individuals, regardless of their sexual orientation or gender identity.
Citations:
- Center for American Progress. (2018). "Discrimination Prevents LGBTQ People From Accessing Health Care." Link
- National Center for Transgender Equality. (2015). "The Report of the 2015 U.S. Transgender Survey." Link
- National Academies of Sciences, Engineering, and Medicine. (2020). "Understanding the Well-Being of LGBTQI+ Populations." Link
- Levy, B. R., & Heidrich, S. M. (2001). "The Role of Discrimination in the Stress and Health of LGBTQ Individuals." Link
- U.S. Department of Health and Human Services. (2021). "HHS Announces Prohibition on Sex Discrimination Includes Discrimination on the Basis of Sexual Orientation and Gender Identity." Link
- Lambda Legal. (n.d.). "Know Your Rights: Healthcare." Link
- Human Rights Campaign. (n.d.). "Healthcare Equality Index." Link














 Ragina Ireland has been lovingly supported throughout her cancer journey by her sister, Johnnie Ireland. Four years ago, Ragina took a Cancer Genetic Risk Assessment test to help give her sister a clearer understanding of her own risk for developing breast cancer.
Ragina Ireland has been lovingly supported throughout her cancer journey by her sister, Johnnie Ireland. Four years ago, Ragina took a Cancer Genetic Risk Assessment test to help give her sister a clearer understanding of her own risk for developing breast cancer. 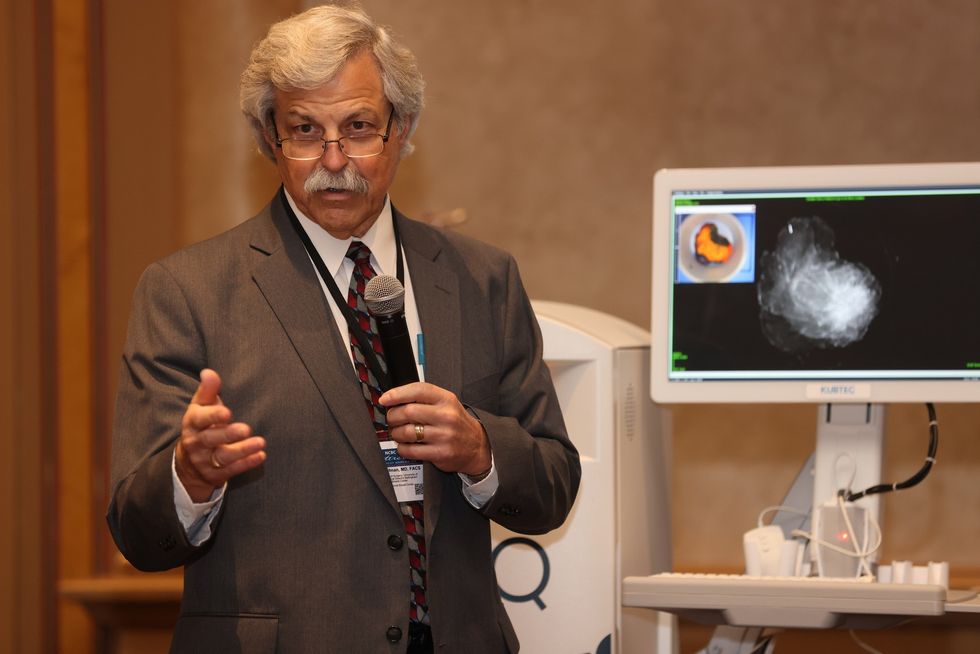 Dr. Cary S. Kaufman teaches the "Essentials of Oncoplastic Surgery" course through the National Consortium of Breast Centers, providing breast surgeons around the world with advanced techniques for optimal breast surgery outcomes.
Dr. Cary S. Kaufman teaches the "Essentials of Oncoplastic Surgery" course through the National Consortium of Breast Centers, providing breast surgeons around the world with advanced techniques for optimal breast surgery outcomes.