On Saturday, I finally got to bring my husband home from the hospital. Bringing a loved one home from the hospital is a significant step in their recovery journey. As a caregiver, you’ll play a crucial role in helping them heal, regain strength, and adjust to life at home. However, transitioning from a hospital setting to home can be overwhelming without the right information and preparation. It's ok to be nervous about bringing your loved one home, but there are some important things to know to help you through this new part of the journey.
1. Understand the Discharge Plan
- Review Instructions Carefully: Hospitals provide a discharge plan that outlines specific instructions for at-home care, medications, follow-up appointments, and lifestyle recommendations. Carefully read through this plan and ask questions if anything is unclear.
- Clarify Medication Information: Know what medications your loved one needs, the dosage, potential side effects, and any interactions with other medications or food. Make sure you understand the timing for each medication and if they require food or specific conditions (e.g., taken with water).
- Learn About New Equipment: If the patient requires equipment, such as oxygen tanks, wheelchairs, or home monitors, get a demonstration on how to use it. Make sure you know who to contact for repairs, maintenance, or troubleshooting.
2. Create a Safe and Comfortable Environment
- Adjust the Living Space: Set up the area where your loved one will spend most of their time to ensure it’s safe, comfortable, and accessible. Remove trip hazards, add grab bars if needed, and arrange for a bed or recliner for easy rest.
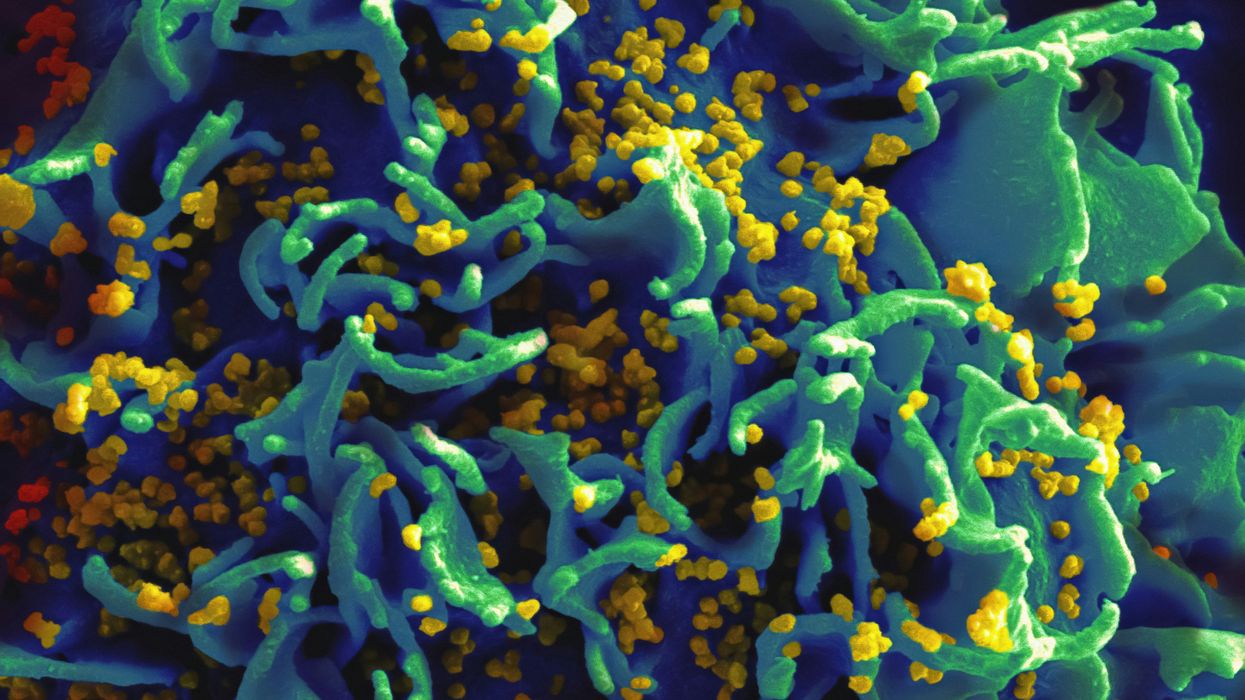
- Ensure a Clean and Organized Home: A clean environment helps reduce infection risk, especially if your loved one has a weakened immune system. Ensure surfaces are sanitized, and essential items (like medications, water, and phone) are within reach.
- Optimize for Accessibility: If mobility is an issue, consider rearranging furniture or setting up a temporary living area on the main floor to avoid stairs. Install nightlights in hallways and bathrooms for safe navigation at night.
3. Know the Signs of Potential Complications
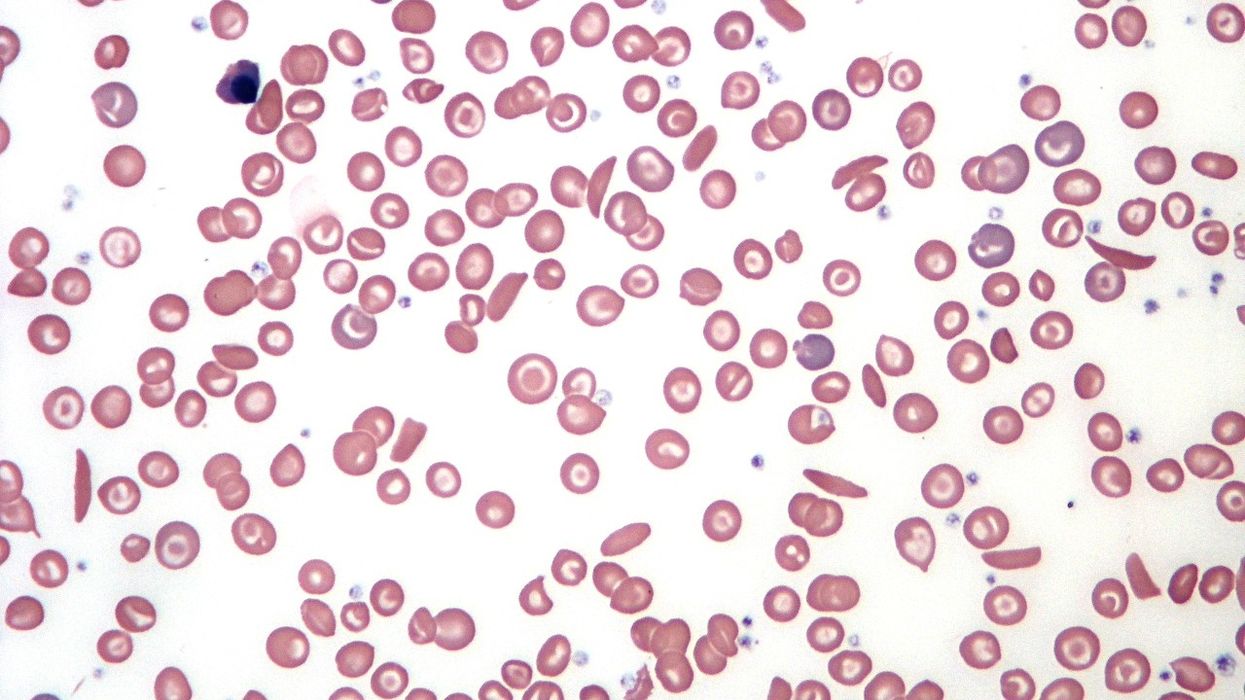
- Monitor for Symptoms: Watch for signs that require medical attention, such as difficulty breathing, excessive bleeding, changes in mental state, severe pain, or infection symptoms (fever, chills, increased redness or swelling at the incision site).
- Keep a Log: Maintain a record of vital signs, medications taken, and any symptoms or side effects. This can be valuable information for follow-up appointments and in case of emergencies.
- Emergency Plan: Ensure you have a clear understanding of who to call in case of an emergency. Save numbers for your loved one’s primary doctor, specialists, the nearest hospital, and any home health service providers.
4. Coordinate Follow-Up Care
- Arrange for Appointments: Discharge instructions often include follow-up appointments. Schedule these appointments as soon as possible, and make a plan for transportation if needed.
- Consider Home Health Services: Depending on the level of care your loved one requires, it may be beneficial to arrange for a visiting nurse, physical therapist, or other home health professionals. Some hospitals can help coordinate these services.
- Stay Connected with Healthcare Providers: Keep in touch with your loved one’s doctors and inform them of any changes in their condition. You might need to advocate on their behalf and ensure they receive appropriate, timely care.
5. Support Physical and Emotional Recovery
- Encourage Physical Activity: If allowed, gentle movement and exercise can help with recovery and prevent complications like blood clots. Follow any physical therapy or mobility guidelines provided.
- Provide Emotional Support: The transition home can be emotionally challenging. Feelings of frustration, anxiety, and sadness are common. Be patient and offer a listening ear. Encourage activities that bring joy, like reading, watching favorite shows, or spending time outdoors.
- Maintain a Healthy Routine: Help your loved one establish a daily routine that includes balanced meals, adequate rest, and social interaction if possible. Regular routines can provide comfort and aid recovery.
6. Look After Yourself as a Caregiver
- Prioritize Self-Care: Caring for a loved one can be physically and emotionally demanding. Remember to take breaks, rest, and maintain a healthy lifestyle for yourself. It’s okay to ask for help when you need it.
- Build a Support Network: Don’t be afraid to reach out to family members, friends, or local support groups for caregivers. Sharing the responsibility can help prevent burnout and provide a sense of community.
- Seek Professional Help If Needed: If caring for your loved one becomes overwhelming, consider hiring a professional caregiver, even if it’s just for a few hours a week. This can give you time to recharge and handle other responsibilities.
7. Manage Finances and Paperwork
- Understand Insurance and Billing: Review any bills from the hospital stay and follow up with the insurance provider if you have questions. Ensure you understand what is covered for follow-up care, medications, and home health services.
- Prepare Legal Documents: Check if there’s a need for legal documents, such as a medical power of attorney, in case your loved one cannot make healthcare decisions. Ensure all necessary documents are up-to-date and accessible.
8. Encourage and Practice Open Communication
- Discuss Recovery Goals: Talk to your loved one about their goals and expectations for recovery. Understanding their hopes and concerns can make the process smoother and keep you both on the same page.
- Set Realistic Expectations: Recovery can take time, and progress may vary. Celebrate small milestones and keep the focus on gradual improvement rather than immediate results.
Transitioning from hospital to home requires patience, planning, and compassion. There were plenty of things I didn't realize I would need to do, but by following these steps, you can create a supportive environment that encourages healing and enhances the quality of life for your loved one. Remember, you’re not alone in this journey. With the right tools, resources, and a caring attitude, you can make this experience as positive and comfortable as possible. You are strong! You are important! You are a caregiver!