In recent years, there has been increasing interest in understanding the impact of gender on medical practice, particularly concerning the performance of women doctors. Despite progress towards gender equality in medicine, stereotypes and biases persist regarding the abilities and effectiveness of female physicians. But the question remains: Are women doctors better?
Clinical Competence and Quality of Care:
Numerous studies have investigated the clinical competence and quality of care provided by women doctors compared to their male counterparts. Contrary to prevailing stereotypes, research consistently demonstrates that there is no significant difference in the clinical outcomes or quality of care delivered by women and men physicians (Tsugawa et al., 2017). Studies examining patient mortality rates, complication rates, and adherence to clinical guidelines have found no substantial disparities based on physician gender (Morgan et al., 2019).
Communication and Patient Satisfaction:
Effective communication is essential in healthcare delivery and can significantly impact patient satisfaction and outcomes. Research suggests that women doctors may possess certain communication skills that contribute to positive patient experiences. Studies have found that female physicians tend to engage in more patient-centered communication, display greater empathy, and spend more time with patients during consultations compared to male physicians (Roter & Hall, 2004). As a result, patients may perceive women doctors as more attentive, caring, and approachable.
Diversity and Representation:
The presence of women in medicine has important implications for diversity and representation in healthcare. Women doctors bring unique perspectives, experiences, and insights to patient care, which can enhance cultural competence and improve healthcare outcomes for diverse patient populations (Burgess et al., 2020). Furthermore, increasing the representation of women in leadership positions within the medical profession can help address gender disparities and promote equity in healthcare delivery.
Challenges and Bias:
Despite the evidence supporting the competence and effectiveness of women doctors, they continue to face challenges and biases within the medical profession. Gender-based discrimination, implicit bias, and stereotypes persist, affecting women’s career advancement, pay equity, and professional recognition (Fileborn et al., 2021). Addressing these systemic barriers and promoting gender equity in medicine remains an ongoing endeavor.
The notion that women doctors are inherently better or worse than their male counterparts is a simplistic and unfounded stereotype. Empirical evidence consistently demonstrates that there is no significant difference in the clinical competence or quality of care provided by women and men physicians. Instead of perpetuating gender-based stereotypes, it is crucial to recognize and celebrate the diversity of experiences and perspectives within the medical profession. By promoting gender equity, addressing bias and discrimination, and fostering inclusive environments, we can ensure that all physicians, regardless of gender, have the opportunity to thrive and deliver high-quality care to their patients.
References:
- Tsugawa, Y., Jena, A. B., Figueroa, J. F., Orav, E. J., Blumenthal, D. M., & Jha, A. K. (2017). Comparison of hospital mortality and readmission rates for Medicare patients treated by male vs female physicians. JAMA internal medicine, 177(2), 206-213.
- Morgan, A. U., Ingraham, A. M., & Arora, V. M. (2019). Does physician gender affect satisfaction and patient experiences in healthcare? A systematic review. PloS one, 14(7), e0220876.
- Roter, D. L., & Hall, J. A. (2004). Physician gender and patient-centered communication: A critical review of empirical research. Annual review of public health, 25, 497-519.
- Burgess, D. J., Phelan, S., Workman, M., Shireman, T. I., & Brown, M. T. (2020). Evaluation of patient-rated and objectively measured physician empathy across demographic groups. Journal of general internal medicine, 35(9), 2641-2648.
- Fileborn, B., Power, J., Flynn, A., Brown, G., Lyons, A., Hinchliff, S., … & Hinchliff, S. (2021). The health and wellbeing of women in medicine: A scoping review. BMC public health, 21(1), 1-17.














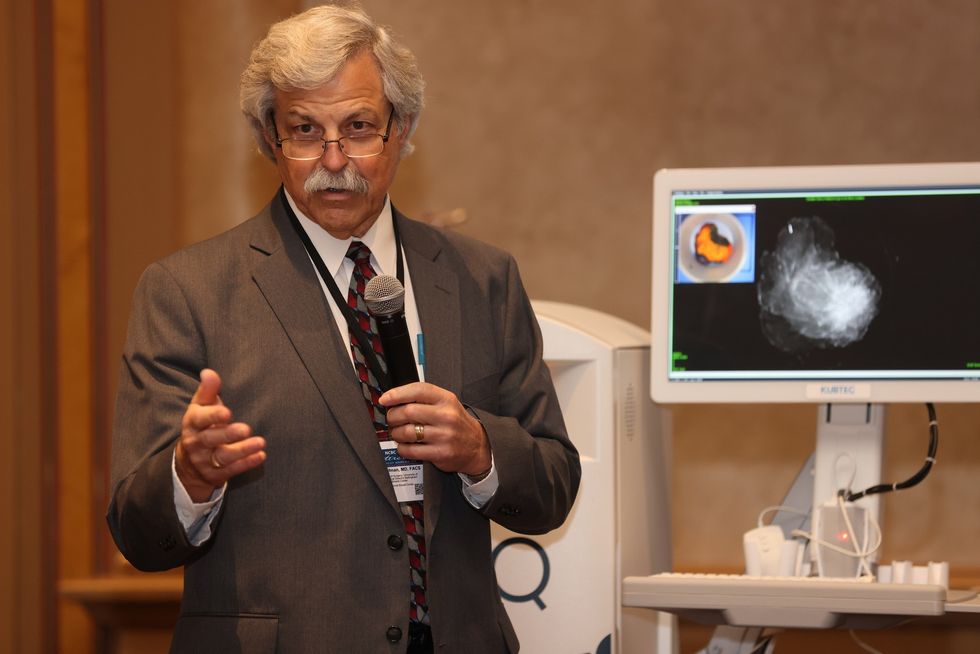 Dr. Cary S. Kaufman teaches the "Essentials of Oncoplastic Surgery" course through the National Consortium of Breast Centers, providing breast surgeons around the world with advanced techniques for optimal breast surgery outcomes.
Dr. Cary S. Kaufman teaches the "Essentials of Oncoplastic Surgery" course through the National Consortium of Breast Centers, providing breast surgeons around the world with advanced techniques for optimal breast surgery outcomes.

