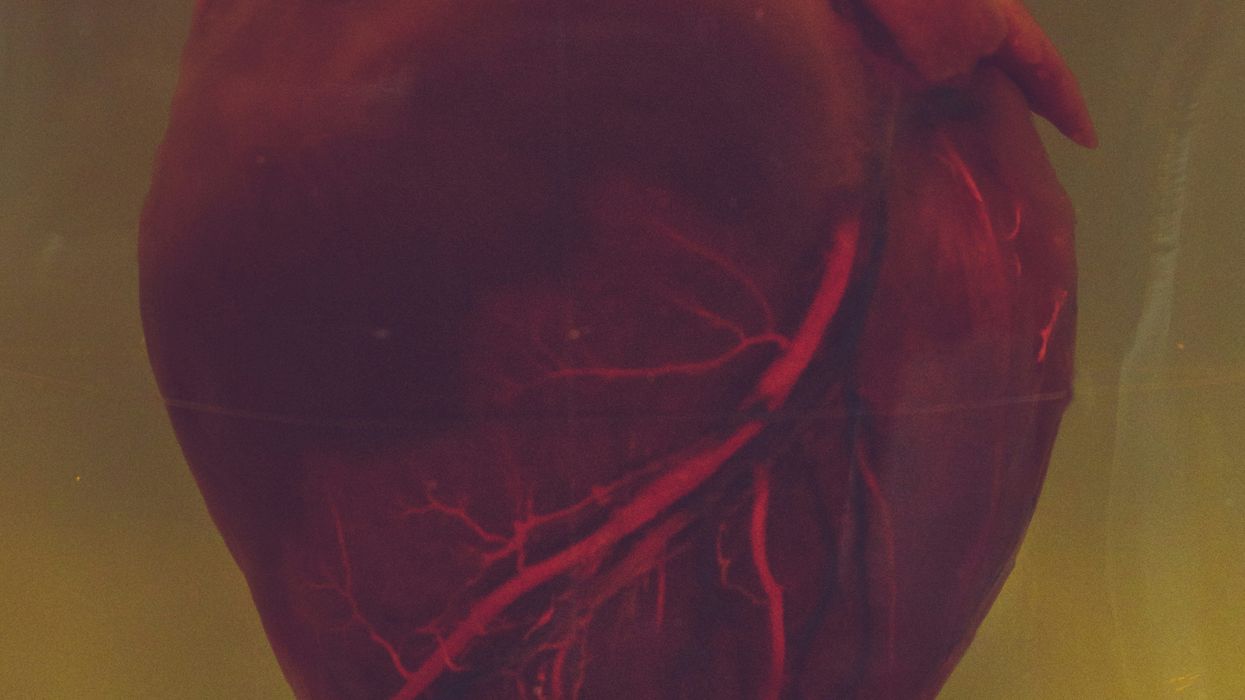
A recent study has highlighted a concerning link between unhealthy behaviors prevalent in lower-income populations and an increase in coronary artery disease (CAD). This trend emphasizes the urgent need for targeted public health interventions to address the social determinants of health that disproportionately affect these communities.
Understanding the Link Between Unhealthy Behaviors and Coronary Artery Disease
Coronary artery disease, the most common form of heart disease, is a condition where the coronary arteries narrow due to plaque buildup, limiting blood flow to the heart. This leads to an increased risk of heart attacks, strokes, and other cardiovascular complications. Risk factors for CAD include smoking, poor diet, lack of physical activity, and conditions like hypertension and diabetes.
Lower-income populations are disproportionately affected by these risk factors due to a variety of socioeconomic and environmental barriers. The study revealed that behaviors such as smoking, poor nutrition, and physical inactivity are more common in communities with limited access to healthy food, healthcare, and safe recreational spaces. According to the American Heart Association, socioeconomic status plays a critical role in shaping health behaviors and outcomes, making lower-income individuals more vulnerable to heart disease.
The Role of Social Determinants of Health
Social determinants of health—conditions in the environments where people live, learn, work, and play—significantly impact health outcomes. Factors such as education level, employment status, income, and access to healthcare services are all key determinants of an individual's ability to engage in healthy behaviors.
In lower-income communities, there is often limited access to fresh fruits and vegetables, recreational facilities, and healthcare services, making it more difficult for individuals to maintain a healthy lifestyle. Food deserts, areas where healthy, affordable food is scarce, are common in these regions, forcing many to rely on fast food or processed options high in sugar, fat, and salt—factors that directly contribute to heart disease.
Moreover, stressors related to financial instability, job insecurity, and unsafe neighborhoods can exacerbate unhealthy behaviors. Chronic stress, combined with a lack of resources, leads to higher rates of smoking and substance abuse as coping mechanisms. Research published in The Lancet points to these environmental stressors as major contributors to the higher incidence of CAD in lower-income populations(
ScienceDaily).The Need for Targeted Public Health Interventions
To reduce the incidence of coronary artery disease in lower-income communities, targeted public health interventions must address the underlying social determinants of health. This includes:
- Improving Access to Healthcare
Lower-income individuals often lack access to quality healthcare due to financial barriers or geographic isolation. Expanding Medicaid and other forms of subsidized health insurance can help these populations access preventive care, including regular check-ups and screenings for heart disease risk factors like high blood pressure and cholesterol levels. - Promoting Healthy Food Access
Addressing food deserts by encouraging the establishment of grocery stores in underserved areas, supporting community gardens, and providing nutrition education are crucial steps toward improving dietary habits. Initiatives like the USDA's Healthy Food Financing Initiative aim to increase the availability of healthy, affordable food in underserved communities, helping to reduce CAD risk factors like poor diet. - Creating Safe Spaces for Physical Activity
Ensuring that lower-income communities have access to safe, well-maintained parks and recreational spaces is vital for promoting physical activity. Cities can also implement infrastructure changes, such as adding bike lanes and pedestrian-friendly walkways, to encourage exercise in urban areas. - Tackling Smoking and Substance Abuse
Tobacco use is one of the leading risk factors for coronary artery disease, and it remains more prevalent in lower-income communities. Public health campaigns aimed at reducing smoking through education, increased taxes on tobacco products, and access to smoking cessation programs are essential. Similar approaches should be taken to address substance abuse, which is often exacerbated by socioeconomic stressors.
Policy Changes and Community-Based Approaches
Government policies that target social and economic inequalities are critical for reducing health disparities. Expanding healthcare coverage, raising the minimum wage, and improving access to education can all play a role in reducing the risk of heart disease in lower-income populations. Moreover, community-based approaches that involve local leaders and organizations can tailor interventions to meet the unique needs of each community, making them more effective.
Public health agencies should also focus on culturally relevant health promotion strategies, recognizing that different communities may require different approaches. For example, interventions in predominantly Black or Latino communities should be designed with cultural sensitivities in mind to ensure higher participation and effectiveness.
The recent study linking unhealthy behaviors among lower-income populations to higher rates of coronary artery disease underscores the urgent need for targeted public health interventions. Addressing social determinants of health, such as access to nutritious food, safe spaces for physical activity, and affordable healthcare, is crucial for reducing the burden of heart disease in these communities. Policymakers, healthcare providers, and community leaders must collaborate to create sustainable, equitable solutions that promote heart health and overall well-being.
Sources:
- American Heart Association. Socioeconomic Factors and Heart Disease. Retrieved from heart.org.
- The Lancet. (2024). Impact of Socioeconomic Stressors on Heart Disease. Retrieved from thelancet.com.
- ScienceDaily. (2024, September 17). Unhealthy Behaviors Contribute to More Coronary Artery Disease Deaths in the Poor. Retrieved from sciencedaily.com(ScienceDaily).








 Karla Mingo believes that her greatest gift as a cancer survivor is the ability to live with gratitude and thankfulness.
Karla Mingo believes that her greatest gift as a cancer survivor is the ability to live with gratitude and thankfulness.