The doctor-patient relationship is a cornerstone of healthcare, characterized by trust, communication, and understanding. In recent years, there has been growing interest in the concept of concordance, which refers to the alignment of certain demographic characteristics between doctors and their patients, such as race, religion, gender, or sexual orientation. Finding a doctor you are comfortable with is significant but it is important to think about surrounding doctor-patient concordance and its potential impact on healthcare outcomes and patient experiences.
Race and Ethnicity Concordance:
Research suggests that race and ethnicity concordance between doctors and patients can have significant implications for healthcare delivery. Studies have shown that patients of color are more likely to report feeling understood and respected when they see a healthcare provider who shares their racial or ethnic background (Saha et al., 2000). Concordance has also been associated with higher levels of patient satisfaction, better communication, and increased adherence to medical recommendations (Cooper et al., 2003).
Religious Concordance:
While less studied than race and ethnicity concordance, religious alignment between doctors and patients may also influence healthcare experiences. Patients may feel more comfortable discussing sensitive issues related to their religious beliefs, values, or practices with a healthcare provider who shares their faith. This shared understanding can foster trust and empathy, ultimately enhancing the quality of care (Ghazi et al., 2018).
Gender Concordance:
Gender concordance between doctors and patients can play a role in healthcare interactions, particularly in specialties where gender-related issues are prominent, such as gynecology or urology. Some patients may feel more at ease discussing intimate or gender-specific concerns with a healthcare provider of the same gender, leading to improved communication and patient satisfaction (Roter et al., 2002).
Sexual Orientation Concordance:
For LGBTQ+ individuals, seeing a healthcare provider who is knowledgeable about and sensitive to their unique healthcare needs is crucial. Research suggests that LGBTQ+ patients may experience discrimination or discomfort when seeking healthcare, particularly if their provider lacks understanding of LGBTQ+ issues. Concordance in sexual orientation can help mitigate these barriers and foster a more supportive healthcare environment (Martos et al., 2020).
While the concept of doctor-patient concordance remains complex and multifaceted, evidence suggests that shared identity factors such as race, religion, gender, and sexual orientation can influence healthcare experiences and outcomes. Patients may feel more understood, respected, and supported when they see a healthcare provider who shares certain demographic characteristics with them. However, it is essential to recognize that concordance is just one aspect of the doctor-patient relationship, and factors such as clinical competence, empathy, and cultural competence are equally important. Moving forward, efforts to promote diversity, equity, and inclusion in healthcare settings can help ensure that all patients receive high-quality, patient-centered care, regardless of demographic differences.
References:
- Saha, S., Komaromy, M., Koepsell, T. D., & Bindman, A. B. (2000). Patient-physician racial concordance and the perceived quality and use of health care. Archives of Internal Medicine, 160(15), 2189-2196.
- Cooper, L. A., Roter, D. L., Johnson, R. L., Ford, D. E., Steinwachs, D. M., & Powe, N. R. (2003). Patient-centered communication, ratings of care, and concordance of patient and physician race. Annals of Internal Medicine, 139(11), 907-915.
- Ghazi, A., Zipp, S., Roth, A., & Hattab, C. (2018). The effect of religious concordance on patient satisfaction, duration of visit, and adherence in surgical and rehabilitation patients. Journal of religion and health, 57(6), 2392-2402.
- Roter, D. L., Hall, J. A., Aoki, Y., & Physician Gender, Patient Gender, and Primary Care. (2002). Physician Gender, Patient Gender, and Primary Care. Journal of Women’s Health & Gender-Based Medicine, 9(7), 769-777.
- Martos, A. J., Nezhad, S., & Morris, N. (2020). Sexual orientation and transgender identity disclosure to healthcare providers: Patient experiences and preferences. LGBT health, 7(3), 129-136.









 Karla Mingo believes that her greatest gift as a cancer survivor is the ability to live with gratitude and thankfulness.
Karla Mingo believes that her greatest gift as a cancer survivor is the ability to live with gratitude and thankfulness.


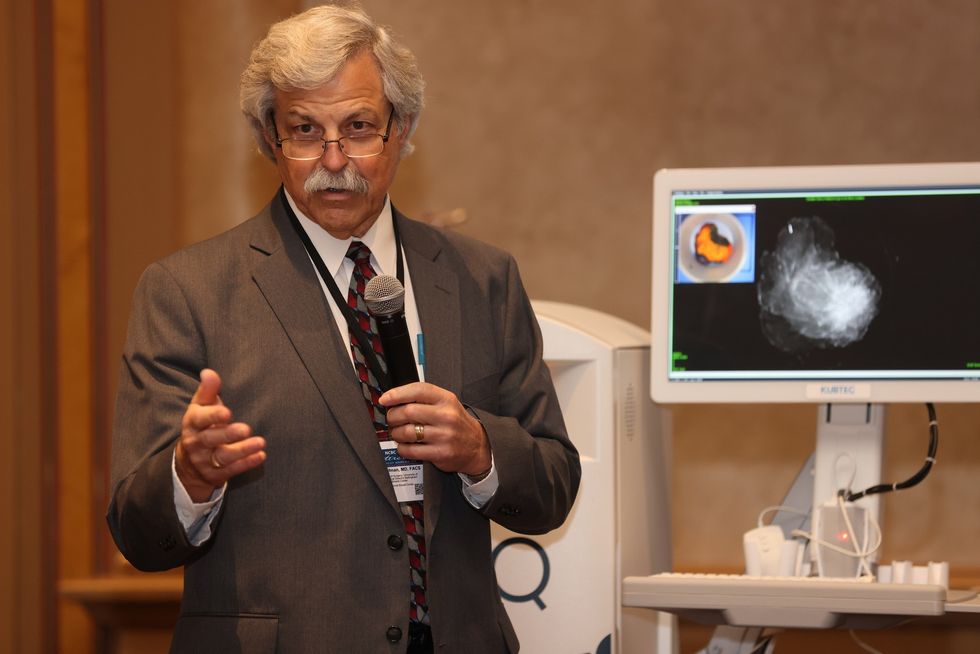 Dr. Cary S. Kaufman teaches the "Essentials of Oncoplastic Surgery" course through the National Consortium of Breast Centers, providing breast surgeons around the world with advanced techniques for optimal breast surgery outcomes.
Dr. Cary S. Kaufman teaches the "Essentials of Oncoplastic Surgery" course through the National Consortium of Breast Centers, providing breast surgeons around the world with advanced techniques for optimal breast surgery outcomes.