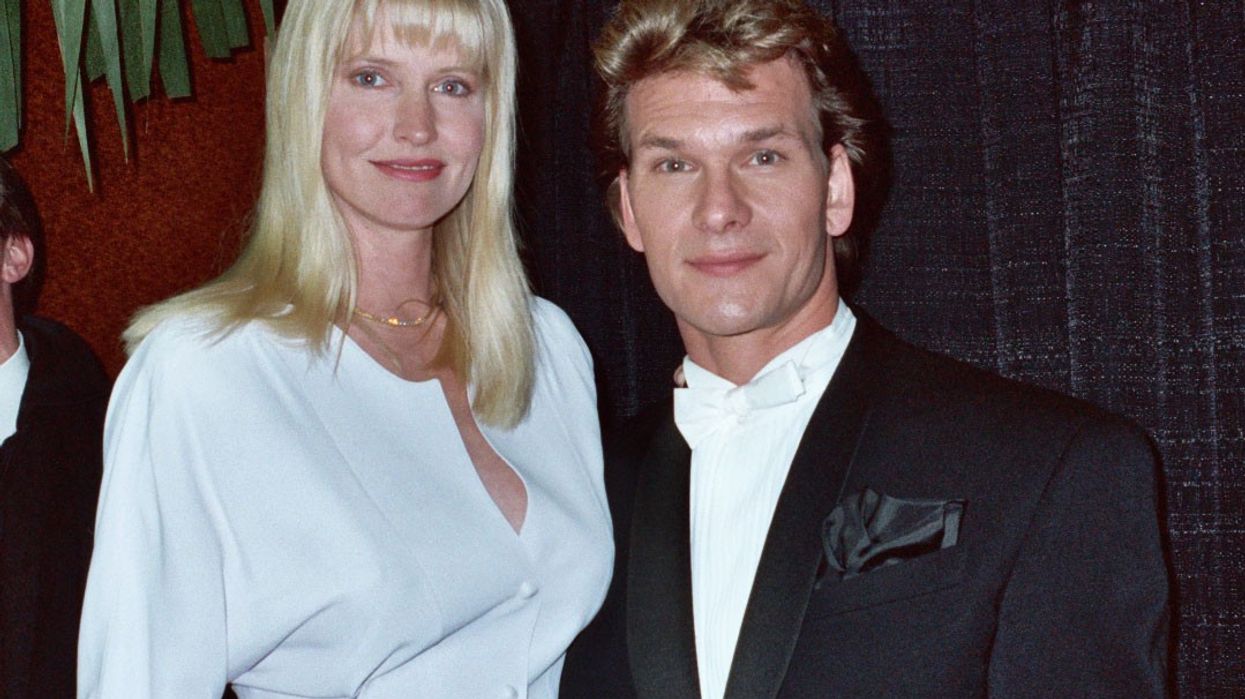
What 80's kid didn't love Patrick Swayze? Johnny Castle, Bohdi, James Dalton, Vida Boheme, and pancreatic cancer patient. Less than two years after he was diagnosed, Patrick Swayze died. Pancreatic cancer is one of the most aggressive and challenging cancers to diagnose and treat, earning a reputation as one of the deadliest forms of cancer. Despite accounting for only about 3% of all cancers in the U.S., it ranks as the fourth leading cause of cancer-related deaths. Its high mortality rate makes it crucial to understand the factors behind its severity and the advancements being made to combat it 【1】【2】.
Why Is Pancreatic Cancer So Deadly?
- Late Diagnosis
Pancreatic cancer is often referred to as a "silent killer" because symptoms usually appear only in advanced stages. Common signs, such as abdominal pain, jaundice, and weight loss, often overlap with other conditions, delaying diagnosis. By the time pancreatic cancer is detected, it has often spread to other organs, making treatment more difficult 【2】【3】. - Aggressive Nature
Pancreatic tumors are highly invasive and have a unique ability to metastasize quickly. The cancer often spreads to the liver, lungs, or surrounding blood vessels, further limiting treatment options 【3】. - Resistance to Treatment
Unlike some cancers that respond well to chemotherapy or radiation, pancreatic cancer is often resistant to these therapies. Its dense tissue environment, called the tumor microenvironment, acts as a barrier, protecting cancer cells from treatment 【4】. - Genetic Complexity
Pancreatic cancer exhibits numerous genetic mutations, which complicates the development of targeted therapies. This genetic diversity makes it challenging to identify universal treatment strategies 【5】. - Low Survival Rates
The five-year survival rate for pancreatic cancer is just 12%, one of the lowest among major cancers. However, early detection can significantly improve outcomes, with localized cases having a five-year survival rate of around 44% 【1】.
What Is Being Done to Improve Treatment?
Despite its challenges, significant progress is being made in pancreatic cancer research and treatment:
- Advances in Early Detection
Researchers are developing blood tests to detect biomarkers associated with pancreatic cancer. Tests for substances like CA19-9, a tumor marker, are being refined for earlier and more accurate diagnosis. Additionally, liquid biopsies, which analyze cancer-related DNA in the blood, are showing promise 【6】【7】. - Improved Imaging Techniques
Enhanced imaging methods, such as endoscopic ultrasound (EUS) and advanced MRI scans, are helping physicians detect smaller tumors and assess the extent of the disease more accurately 【8】. - Targeted Therapies
Targeted treatments like PARP inhibitors, which focus on specific genetic mutations such as BRCA1 and BRCA2, have shown success in subsets of pancreatic cancer patients. These therapies offer a personalized approach and better outcomes 【9】. - Immunotherapy Advances
Immunotherapy, which boosts the body’s immune system to attack cancer cells, is being studied for pancreatic cancer. Clinical trials using immune checkpoint inhibitors and cancer vaccines are ongoing, with some showing encouraging results 【10】. - New Chemotherapy Combinations
While traditional chemotherapy remains a mainstay, combining drugs like FOLFIRINOX (a mix of four chemotherapy agents) has improved survival rates in some patients. This regimen, though intense, offers hope for those with advanced-stage disease 【11】. - Focus on the Tumor Microenvironment
Scientists are working on therapies that disrupt the tumor microenvironment, making it easier for treatments to penetrate and destroy cancer cells. Experimental drugs that target these barriers are currently in clinical trials 【4】.
What Can Be Done to Reduce Risk?
Although not all cases of pancreatic cancer are preventable, lifestyle changes can help lower risk:
- Quit Smoking: Smoking is one of the leading risk factors for pancreatic cancer.
- Maintain a Healthy Weight: Obesity increases the risk of developing this cancer.
- Adopt a Healthy Diet: Diets rich in fruits, vegetables, and whole grains and low in processed meats can reduce cancer risk 【2】.
Additionally, individuals with a family history of pancreatic cancer or genetic predispositions (e.g., BRCA mutations) should consider genetic counseling and regular screenings.
Although pancreatic cancer remains a formidable challenge, advancements in early detection, personalized medicine, and innovative treatments are changing the landscape. Advocacy and funding from organizations like the Pancreatic Cancer Action Network (PanCAN) are driving progress in research and patient support.
Continued collaboration among researchers, clinicians, and advocacy groups offers hope for a future where pancreatic cancer is no longer a deadly diagnosis.
References
- American Cancer Society. (2023). Cancer Facts & Figures. Retrieved from cancer.org.
- National Cancer Institute. Pancreatic Cancer Statistics. Retrieved from cancer.gov.
- Mayo Clinic. Pancreatic Cancer Symptoms and Causes. Retrieved from mayoclinic.org.
- National Institutes of Health (NIH). Tumor Microenvironment in Pancreatic Cancer. Retrieved from nih.gov.
- Johns Hopkins Medicine. Genetic Basis of Pancreatic Cancer. Retrieved from hopkinsmedicine.org.
- PanCAN. Early Detection Research. Retrieved from pancan.org.
- Nature Reviews Clinical Oncology. Advances in Liquid Biopsy Technologies. Retrieved from nature.com.
- Cleveland Clinic. Imaging Techniques for Pancreatic Cancer. Retrieved from clevelandclinic.org.
- FDA. Targeted Therapies for Pancreatic Cancer. Retrieved from fda.gov.
- American Association for Cancer Research. Immunotherapy Trials for Pancreatic Cancer. Retrieved from aacr.org.
- Journal of Clinical Oncology. FOLFIRINOX and Survival in Pancreatic Cancer. Retrieved from ascopubs.org.









 Dr. Jay Harness, MD, FACS, founder of Cancer Fitness, believes that when a woman begins exercising after breast cancer, it marks the start of her personal reconstruction journey.
Dr. Jay Harness, MD, FACS, founder of Cancer Fitness, believes that when a woman begins exercising after breast cancer, it marks the start of her personal reconstruction journey.







