For many breast cancer patients, surviving the disease is just one part of the journey. The path forward often includes physical healing, emotional restoration, and reclaiming one’s sense of self. That’s where oncoplastic surgery is changing the landscape—offering women not only life-saving procedures but also renewed confidence and dignity.
This innovative approach blends oncology (cancer surgery) with plastic and reconstructive techniques, allowing surgeons to remove tumors while reshaping the breast for a more natural appearance. The result? A holistic healing process that honors both survival and self-image.
What Is Oncoplastic Surgery?
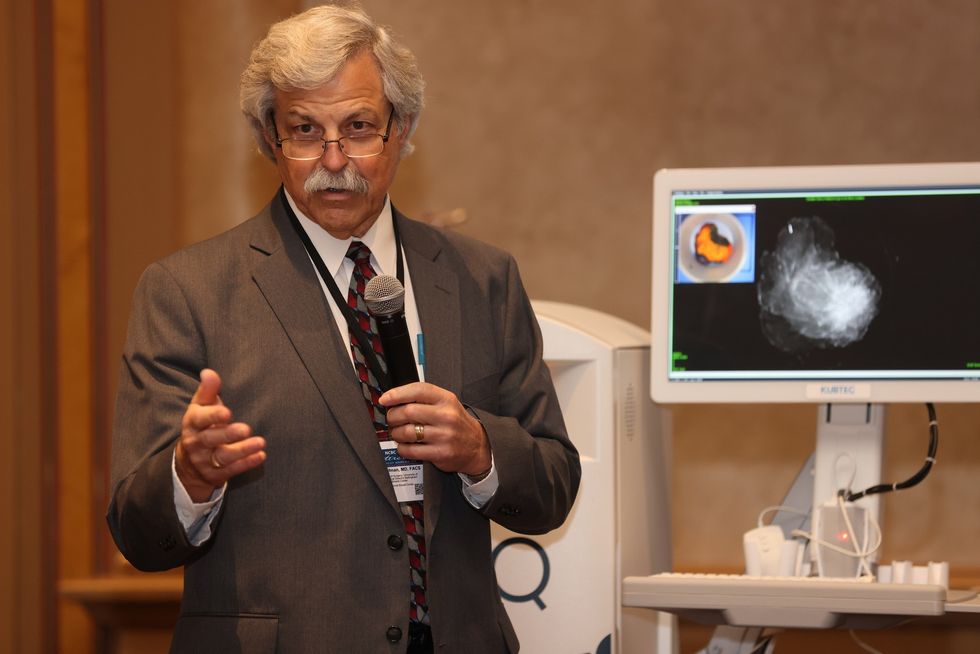
“Curing cancer used to be the sole goal of cancer treatment,” said Dr. Cary S. Kaufman, a breast surgical oncologist in Bellingham, Washington. “As long as we did our best to cure the patient, we had accomplished our goal. But patients want more—they want to live cancer-free and return to a life that feels as close to normal as possible.”
Kaufman, who teaches the Essentials of Oncoplastic Surgery course through the National Consortium of Breast Centers, emphasizes the importance of restoring both health and appearance. “With oncoplastic surgery, we not only treat the cancer but also work to preserve or even improve the natural shape of the breast. That’s a valuable addition to overall care.”
Oncoplastic surgery is typically performed at the time of a lumpectomy (breast-conserving surgery), and in some cases following mastectomy when reconstruction is needed. By integrating aesthetic reconstruction with tumor removal, patients are spared the added trauma of major changes to their body image.
A Shift Toward Whole-Person Healing
Historically, women often had to choose between complete cancer removal and preserving the appearance of their breasts. Oncoplastic surgery eliminates that heartbreaking tradeoff—empowering patients to pursue both survival and quality of life.
“The biggest issue I see—especially among African American women—is access and understanding,” said renowned breast surgeon Dr. Ronda S. Henry-Tillman, who practices in Little Rock, Arkansas. “A woman may be told she needs a mastectomy, but no one explains her options for reconstruction. Sometimes providers themselves aren’t trained or don’t offer those options. That’s a disparity in care, and it’s deeply unfair.”
Oncoplastic surgery doesn’t just reshape the body—it helps heal the mind and spirit. Studies show that women who undergo these procedures report higher satisfaction with their bodies, improved self-esteem, and lower rates of post-treatment depression.
Jennifer Gass, MD, FACS, Director of the Breast Health Center at Brown University stated,
“We conducted a study using the National Surgical Quality Improvement Program (NSQIP) database to look at breast reductions performed at the time of lumpectomy for cancer patients. We found no difference in the rate of oncoplastic procedures between white and Black patients. However, Hispanic patients had fewer oncoplastic procedures, which we interpreted as potentially related to language barriers.
Gass also conducted a separate project that examined how a woman feels about her appearance and well-being after breast surgery. “I believe achieving a good cosmetic outcome positively impacts a woman’s mental health, which in turn supports her overall well-being. Oncoplastic surgery should be accessible to all women,” added Dr. Gass.
Who Is a Candidate for Oncoplastic Surgery?
Oncoplastic techniques are often best suited for patients with moderate to large breasts who are undergoing lumpectomies that require reshaping for symmetry. Some mastectomy patients may also qualify for immediate reconstruction using oncoplastic principles.
The key is early planning. Ideally, patients should meet with a multidisciplinary team that includes a surgical oncologist, plastic surgeon, and breast care navigator. This allows for thoughtful treatment planning and a smoother recovery.
Why Oncoplastic Surgery Matters
“This process is about helping patients feel whole again,” said Dr. Kaufman. “The real reward comes during the follow-up months after surgery—when the patient is standing in front of the mirror, and even the surgeon has trouble telling which breast had the procedure. Can you find the scar? Do they look different? That’s the power of oncoplastic surgery.”
Dr. Kaufman envisions a future where oncoplastic techniques are no longer considered an “add-on,” but simply the standard in breast cancer surgery. “When every breast surgeon incorporates these principles into their work, we won’t need a separate term for it. That’s the future I hope for.”
Access and Advocacy Are Still Needed
Despite its benefits, oncoplastic surgery is not universally accessible. Barriers such as insurance coverage, lack of surgeon training, and limited awareness continue to affect patients—especially in underserved and minority communities.
Breast cancer may leave a mark, but oncoplastic surgery offers survivors a powerful way to reclaim their bodies, their confidence, and their lives. For many women, it represents a turning point—where fear and loss give way to healing, strength, and renewed self-worth.
Because in the end, it's not just about surviving cancer. It's about surviving whole.