For a long time, getting a diagnosis of HIV was devastating. In a remarkable breakthrough, a 7th individual has been reported to potentially be cured of HIV following a stem cell transplant for leukemia. This case underscores the potential of stem cell transplants not only as a treatment for blood cancers but also as a promising approach to achieving an HIV cure.
The Case
The patient, a 53-year-old man from Düsseldorf, Germany, was diagnosed with HIV in 2008 and later developed leukemia. In 2013, he underwent a stem cell transplant using cells from a donor with a rare genetic mutation known as CCR5-delta32. This mutation confers resistance to HIV by preventing the virus from entering and infecting immune cells.
The Science Behind the Cure
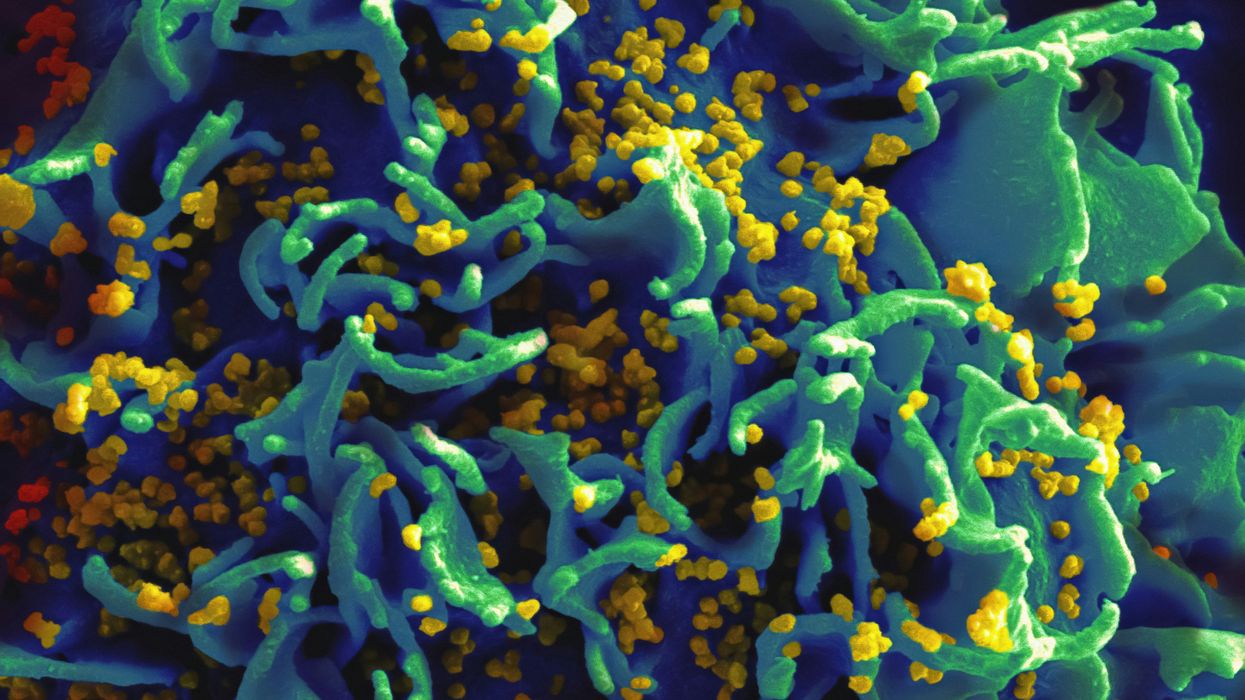
The CCR5-delta32 mutation is a naturally occurring genetic variant that disables the CCR5 receptor on the surface of immune cells. Most strains of HIV use this receptor to enter and infect cells. Individuals with two copies of this mutation are highly resistant to HIV infection.
Stem cell transplants involve replacing a patient's immune cells with those from a healthy donor. In cases where the donor has the CCR5-delta32 mutation, the recipient's new immune cells are similarly resistant to HIV. This method has been previously successful, most notably in the cases of Timothy Ray Brown (the "Berlin Patient") and Adam Castillejo (the "London Patient").
Monitoring and Results
Following the transplant, the patient ceased antiretroviral therapy (ART) in 2018. Extensive testing has since shown no detectable HIV in the patient's body. This includes tests that detect viral genetic material and assays that measure the presence of infectious virus.
The patient's sustained remission without ART strongly suggests that he is cured of HIV. However, researchers caution that it is still early to declare a definitive cure, as HIV can sometimes persist in hidden reservoirs and reemerge. Continued monitoring will be essential to confirm long-term remission.
Implications and Future Directions
While this case is a significant milestone, stem cell transplants are not a feasible cure for HIV on a broad scale due to their high cost, complexity, and associated risks. They are currently reserved for patients with life-threatening blood cancers.
Nonetheless, these findings provide valuable insights for developing more accessible HIV cure strategies. Research is ongoing to explore gene-editing technologies, such as CRISPR, to replicate the effects of the CCR5-delta32 mutation without the need for a transplant. Additionally, studies aim to identify other potential targets and methods to eradicate HIV reservoirs.
The apparent cure of a seventh person with HIV following a stem cell transplant for leukemia marks a pivotal moment in HIV research. While not a universal solution, it opens new avenues for innovative treatment approaches. Continued research and clinical trials are crucial to translate these insights into practical and scalable HIV cures.
References
- Gupta, R. K., Abdul-Jawad, S., McCoy, L. E., et al. (2019). HIV-1 remission following CCR5Δ32/Δ32 haematopoietic stem-cell transplantation. Nature, 568, 244-248.
- Hütter, G., Nowak, D., Mossner, M., et al. (2009). Long-term control of HIV by CCR5 Delta32/Delta32 stem-cell transplantation. New England Journal of Medicine, 360(7), 692-698.
- Yukl, S. A., Kaiser, P., Kim, P., et al. (2018). Challenges in detecting HIV persistence during potentially curative interventions: a study of the Berlin patient. PLoS Pathogens, 14(2), e1007290.














 Dr. Cary S. Kaufman teaches the "Essentials of Oncoplastic Surgery" course through the National Consortium of Breast Centers, providing breast surgeons around the world with advanced techniques for optimal breast surgery outcomes.
Dr. Cary S. Kaufman teaches the "Essentials of Oncoplastic Surgery" course through the National Consortium of Breast Centers, providing breast surgeons around the world with advanced techniques for optimal breast surgery outcomes.