A breast cancer diagnosis can be life-changing for any woman, but for many women of color, it often comes with additional challenges—limited access to healthcare, cultural and language barriers, and a long history of mistrust toward the medical system.
Why Genetic Testing Matters
“Cancer genetic testing can influence cancer treatment, identify individuals at increased risk, and inform family members about their potential risk,” explains Kim Van Ysseldyk, a Certified Cancer Genetics Practitioner at Sutter Roseville Medical Center in Northern California. “It allows for earlier screenings or preventive surgeries and helps identify patients who meet the guidelines for high-risk care.”
Despite these clear benefits, the National Institutes of Health reports that awareness of genetic testing remains lowest among minority women with breast and ovarian cancer. For example, while Black women have a 4% lower chance of developing breast cancer than white women, their death rate from the disease is 40% higher. Additionally, Black women are more likely to be diagnosed with breast cancer before age 50 and are at a higher risk of developing triple-negative breast cancer, which is associated with several genes related to hereditary breast cancer, including BRCA1, BRCA2, PALB2, and RAD51D.
Barriers Facing Minority Women
Communities of color are significantly underrepresented in genetic counseling and testing, a disparity that Van Ysseldyk is acutely aware of in her work. She and her team take deliberate steps to bridge this gap.
“Our health system has strong relationships with both local and national cancer organizations. Clinicians and staff participate in various events each year to educate and raise awareness about cancer prevention, screening, and cancer care at local cancer support groups, community health fairs, and regional events,” she says.
In the clinic, Van Ysseldyk is mindful of the unique needs of each patient, especially when there is a language barrier or when complex genetic information requires more time to explain. “I encourage family members or caregivers to attend the appointment as well,” she says. “I also use pictures and charts to explain the intricacies of cancer genetics, inheritance patterns, and the testing process. My goal is to foster open communication and build trust with patients. I always tell them that my door is open for any questions or concerns.”
To ensure clear communication, Van Ysseldyk utilizes on-demand video interpretation services or in-person translators when English is not the patient’s primary language. “Since genetic testing affects not only the patient but also their family members, it’s crucial that patients fully understand the process and have the opportunity to ask questions before proceeding,” she explains.

The Genetic Counseling Process
Genetic counseling typically begins with a referral, often from a breast imaging department, surgeon, oncologist, or primary care doctor. The initial appointment involves a detailed review of the patient’s family history and an in-depth discussion about genetic and hereditary cancer risks.
If genetic testing reveals a mutation in BRCA1/2 or another breast cancer gene, it can have immediate implications for breast cancer screening or treatment. Women with inherited mutations may qualify for additional screenings such as annual breast MRIs, in addition to regular mammograms. In some cases, risk-reducing surgeries, like a bilateral mastectomy, may be recommended for patients with a very high-risk gene like BRCA1/2.
Improving Access for Breast Cancer Patients
“We’ve recently expanded our Breast Cancer Nurse Navigation staff,” says Van Ysseldyk.
“These nurses are often the first point of contact for newly diagnosed patients and provide ongoing support throughout their treatment.” Nurse navigators play a crucial role in connecting underinsured or uninsured patients to cancer services, especially those facing significant barriers to care.
The Impact of Lived Experience
Ragina Ireland, a 15-year breast cancer survivor, didn’t have access to genetic testing when she was first diagnosed. However, four years ago, her gynecologist helped her get tested. “I did it for my sister,” says Ireland, who is now an advocate for early detection within the African American community. “With our higher mortality rates, we need answers—and genetic testing could be a key factor in reducing those numbers.”
While Ireland’s test results came back negative, it brought her peace of mind. “It was a relief. However, since I didn’t have a family history, I still worry for my sister.”
Understanding Risk
The National Comprehensive Cancer Network Guidelines recommend cancer genetic counseling for individuals with the following risk factors:
- Breast cancer diagnosed before age 50 or in both breasts.
- Triple-negative breast cancer.
- Ovarian, pancreatic, or male breast cancer diagnosed at any age.
- Breast cancer with Ashkenazi Jewish ancestry.
- A family history of breast cancer or other hereditary cancers like ovarian or prostate cancer.
- A family member with a BRCA1/2 mutation or other hereditary cancer genes such as PALB2, ATM, CHEK2, PTEN, CDH1, or TP53.
Moving Toward Health Equity
Improving access to genetic testing for minority women is not only crucial for better health outcomes—it’s essential for achieving health equity.
“As we learn more about an individual’s genetic results and risk factors, their plan of care can vary significantly,” says Van Ysseldyk. “For high-risk women, annual breast MRIs, along with mammograms, can identify early-stage breast cancer, which has a much higher cure rate.”









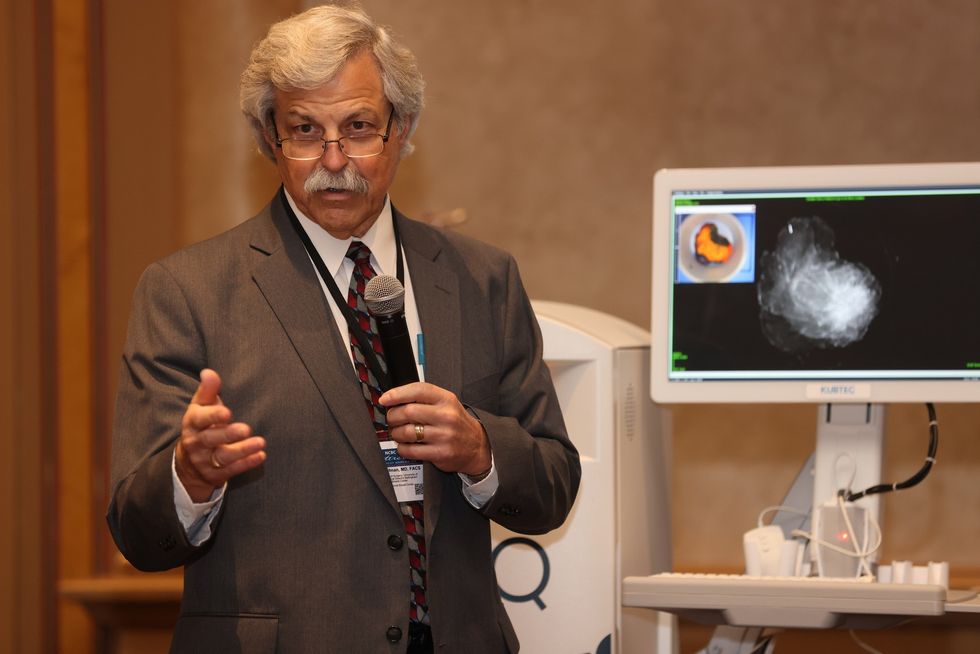 Dr. Cary S. Kaufman teaches the "Essentials of Oncoplastic Surgery" course through the National Consortium of Breast Centers, providing breast surgeons around the world with advanced techniques for optimal breast surgery outcomes.
Dr. Cary S. Kaufman teaches the "Essentials of Oncoplastic Surgery" course through the National Consortium of Breast Centers, providing breast surgeons around the world with advanced techniques for optimal breast surgery outcomes.




 Dr. Jay Harness, MD, FACS, founder of Cancer Fitness, believes that when a woman begins exercising after breast cancer, it marks the start of her personal reconstruction journey.
Dr. Jay Harness, MD, FACS, founder of Cancer Fitness, believes that when a woman begins exercising after breast cancer, it marks the start of her personal reconstruction journey.

