Caregiving is a role that few are prepared for. It demands patience, resilience, and a kind of selflessness that can be all-consuming. I never thought of myself as a natural caregiver, and yet, life has put me in this role time and time again. I previously identified with the scene in 30 Rock when Liz is sick and Jack’s idea of making her feel better is to rub her back with a broom. It’s not that I don’t love and care for the people in my life. I have nieces and a nephew that I would literally do anything for. If they needed a heart to live, I’d give them mine. I have four dogs that I would mortgage my house for, but in 2017 something in me changed.
I met my friend Nina in 2014 through my best friend’s boyfriend. The four of us became a little best friend family. She was my girl bestie… my “nestor,” as I called her. In early 2016 we found out that Nina had cervical cancer. She was going to have a radical hysterectomy to remove the cancer and then we were all going to move on with our lives. When they went to do the surgery, they found that the cancer had spread. She started radiation and chemo immediately. By October of 2016 the doctors declared Nina cancer free. On New Year’s Eve we celebrate that 2016 was the year Nina beat cancer and we were going to move into 2017 healthy and ready to take on the world. By New Year’s Eve 2017, Nina had passed away from cervical cancer.
In April of 2017 Nina started having pain when she would take a deep breath. She went to the doctor and found her lungs were filled with fluid, the cancer was back, and it was terminal. Nina lost her parents when she was young. Her brother and sister lived in Florida, so we were her family. At first it was really just making sure she got to her doctor’s appointment, bringing her to chemo, going to the pharmacy for her… the basics. By the time she died, I was feeding her, showering her, carrying barf bags in my purse… fully taking care of all of her needs. Eventually it got to the point that I was no longer equipped to care for her. She had a cousin and aunt in Pennsylvania who she moved in with. Her aunt was retired and was able to spend every minute with Nina. By the time the end came a once beautiful, bubbly, woman who was the embodiment of sunshine, became weak and you could see that light leaving her. After she died was when I realized I was what someone would refer to as “a caregiver.” It was a job I was thrown into and didn’t know if I could ever do again.
In the midst of Nina’s battle with cervical cancer I was also going through a divorce. After doing a lot of work on myself, in 2019 I met my husband. Our relationship took a strange turn in 2020 when we were quarantined together. We quietly got married on August 21st, 2020. Despite the world being shut down because of Covid, we were living a happy life. On July 4th of 2021 Scott mentioned having a stomach ache. It kept getting worse and one night he went to urgent care. They told him it was constipation and to take Miralax. At 4:00am on July 7th Scott tried to get up to get ready for work, but was in so much pain, he couldn’t stand up straight. We went to the ER. They did blood tests, took x-rays, and a CT scan. A PA came in at some point and said it was kidney stones and said they would work on controlling the pain. At around 7am the ER doctor came in and said he actually thought this was something called GIST cancer, and Dr. Gordon, an oncological surgeon would be coming in to talk to us. I froze. Cancer. That disease that killed my best friend. My husband of less than a year had cancer. I admit, I completely fell apart. Scott was admitted to the hospital to manage the pain and do a biopsy. As I sat in bed alone that night, I realized I was going to be a caregiver again, whether I felt like I could do it or not.
Scott had major abdominal surgery on August 4th. A 12.5 x 9 x 7 cm mass was removed from his intestines and his intestines were resectioned to his bowel. He stayed in the hospital for 6 days, and came home for 3 months of healing. He couldn’t drive for 6 weeks, so I brought him to doctors appointments, did the food shopping, took care of our house, our dogs, our entire life. He started seeing a wonderful oncologist named Dr. Sammartino that had experience with this extremely rare cancer. He was put on an oral targeted therapy medication for 3 years. The process was stressful and took a toll on me, but eventually we got back to our normal lives.
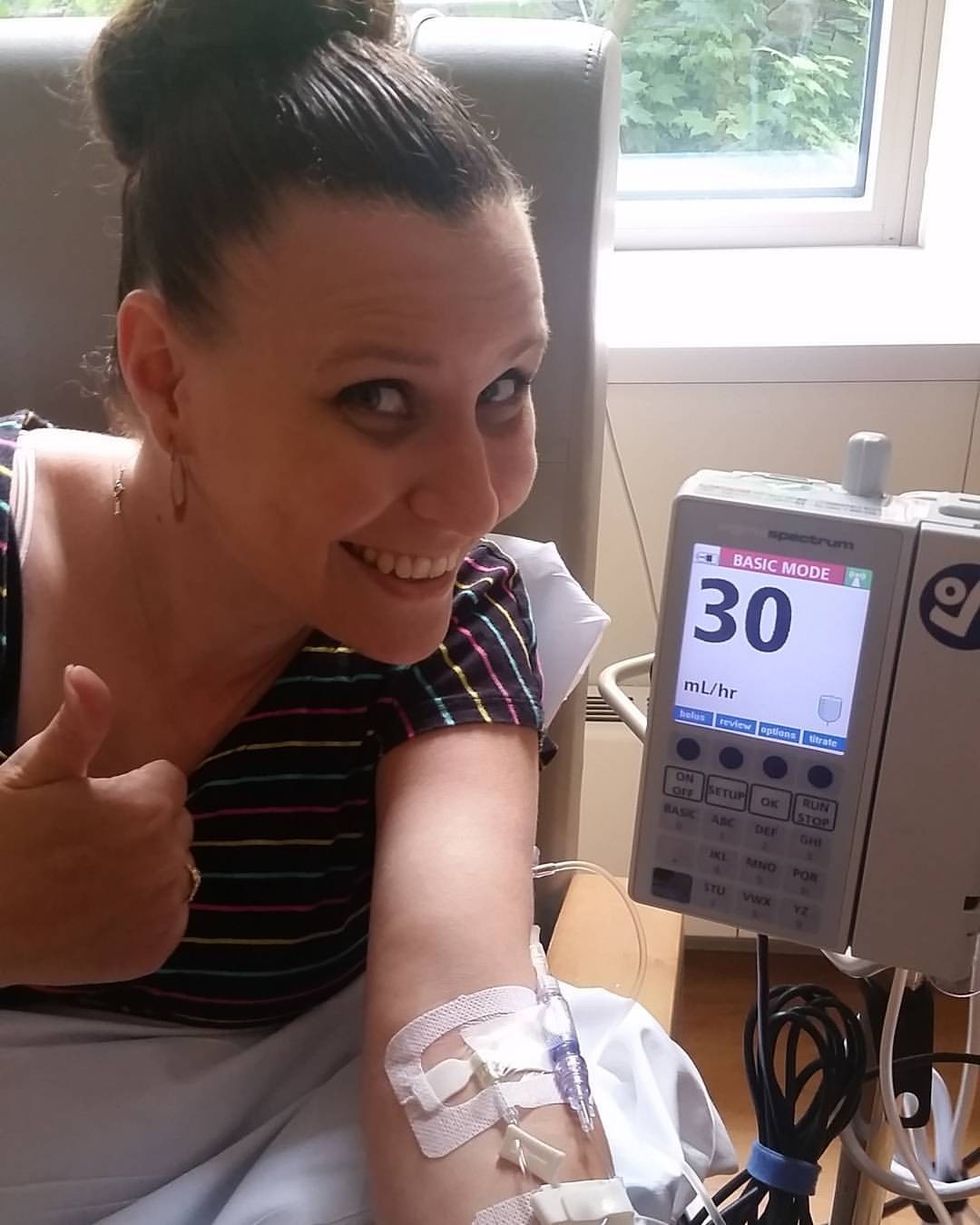
I have chondromalacia, better known as runner’s knee. In March of 2024 I had to have knee surgery. It’s pretty easy surgery. It’s short, you walk out on your own, and everything goes back to normal in a month. Unfortunately, before we could get back to normal Scott started having stomach pains again. We called his oncologist and he told us to go to the emergency room immediately for a CT scan. I felt like I was in the twilight zone. Scott didn’t even have time to get fully checked in before the took him back to a room. They had him drinking contrast for a CT scan within 15 minutes of walking in. It was a Saturday afternoon and we were being treated like we were the only ones in the emergency room. I knew what the outcome of this all was going to be. Eventually, a PA came in and said “the good news is you don’t have a blockage. The bad news is the mass is back.” I was more stunned by the way the PA told us it was back than the fact that it was back. Scott was admitted to the hospital. The next morning Dr. Gordon was standing in Scott’s hospital room telling us we were going to do surgery again the following week. Caregiver mode was activated. Surgery took a long time. It didn’t start till around 4pm and I didn’t get home until 1am. I had trouble getting to sleep knowing everything that was coming. It was the same story as last time. I was Scott’s primary caregiver. I took care of our lives. It was stressful and it took its toll on me again, but this time, our lives didn’t go back to normal.
Scott never felt quite right. He got his three-month CT scan in July but the oncologist had him go back for second CT scan to get more different views. When we went to see Dr. Sammartino to follow-up he said he had discussed Scott’s scans with Dr. Gordon. I knew that if the surgeon was involved in the conversation nothing good was happening. At the beginning of September, we went to see Dr. Gordon. He was concerned enough that he wanted to do another surgery to see what was going on. The plan was to do laprascopic surgery and if he needed to, he would do a full open. So, on Wednesday, September 25th, we went back to the hospital for Scott’s third surgery. They took him back at 11am. I paced around the waiting room for hours. I tried to take my own advice I had written about. I watched a movie, I read a book, I sat and cried. My best friend came and sat with me for a while, and at 7pm Dr. Gordon came out to talk to me. Surgery had gone well, but he had to do a full open and he had to resection Scott’s intestines again. Most of the rest of the night was a blur. I got to see him in recovery, they didn’t have a room for him and I was being kicked out of recovery, so I went home.
That started the longest 18 days of my life. Dr. Gordon had given him an NG tube to give his intestines a break. An NG tube, or nasograstric tube, is stuck in the nose, down the throat, and into the stomach. In Scott’s case, it was to remove his stomach contents. They expected it to be in for a few days, have him eating liquids by the weekend, and the plan was to have him home by Monday or Tuesday. What did Woody Allen say? “If you want to make God laugh, tell Him about your plans.” The first few days seemed to be going according to plan. Scott was up and walking around, he was feeling good, and his spirits were high. But Scott’s intestines decided to take their time moving again. They had started giving him entereg, a drug that helps restore bowel function, while the patient is on opiods. A week after his surgery and a few days-worth of entereg, Scott still wasn’t eating and his intestines weren’t doing anything. All of a sudden there was a concern that there was a blockage in his intestine. Doctors were running in and out of the room and he was scheduled for an emergency CT scan. In a shocking turn of events, there was no blockage and this CT scan showed he was healing well. It was just going to be a matter of waiting for Scott’s intestines to decide to work. The NG tube stayed in.

Over the course of the next few days Scott started feeling better. He was the Floor 5E walking champ. He was watching football games and yelling at the TV over dumb plays. All the normal things Scott would do, only he still wasn’t eating and still had the NG tube in. Two weeks after the surgery the doctors decided to take the NG tube out and Scott was allowed to start on a clear liquid diet. Scott mentioned pain in one of his IV sites, which they checked, but didn’t seem to see anything wrong. Besides, we got him an apple juice and lemon ice now that he could eat again. He started to eat the Italian ices and he said he felt weird and wanted to nap. 15 minutes into his nap he was startled awake and said he felt off. Shortly after that, the nurse tech came in to take Scott’s vitals and noticed he has a small fever of 100 and his heart rate was at 112. The nurse tech waiting a few minutes and to take his vitals again. This time, his fever was 101.4 and his heart rate was at 126. The third time she took it his fever had reached over 103 and his heart rate reached 190. She called a rapid response. All of a sudden, I was being told to leave the room and doctors and nurses came running from all over. I stood on the other side of the floor clutching my computer to my chest. I honestly don’t even know what I had my computer. The last thing I remembering hearing before I ran out was “grab the crash cart now!”
I walked outside still holding my computer close to me. I spoke to my friend Kim to calm me down. We did breathing together. Kim reminded me that Scott was in the right place. He was going to get the help he needed. She then encouraged me to call my best friend Matt. Matt is a paramedic in Westchester County. Not only is he the best of the best, but he also teaches others training to be paramedics. He has a firm understanding of emergency medicine and what may be going on with the emergency situation Scott was in. When it came right down to it, it was all just a distraction. I was scared to go back to his room. I slowly crept back down the halls of 5E. Scott’s nurse spotted me standing in the hall crying, so she came over to explain what had happened. Something was wrong and was causing his temperature to spike and his heart rate to spike. He was immediately put on antibiotics, and on a Blanketrol cooling system to help get his temperature down. They were going to send him for CT scans too. While we were waiting for him to go to his CT scan, Scott told me to go home. My normal schedule was to leave at around 3pm to go home and spend some time with the dogs, feed them, then I’d come back after dinner. On this day, Scott told me to go home at 1pm and told me not to come back for the day. He was right. I needed some time off from the hospital. He had two more rapid responses that day because his fever and heart rate spiked. I did manage to get him into a private room, so we celebrated that win via text and went to bed.
The next day was when we finally started to see a light at the end of the tunnel. The fever spike and heart rate spike were because he had thrombophlebitis in his right arm. Thrombophlebitis happens when a blood clot forms at the site of an inflamed vein. It happens sometimes when someone has an IV in their arm for an extended amount of time. Between the antibiotics and keeping his arm elevated and warm, we really seemed to be turning the corner. The doctor decided to start Scott on full liquids. That meant he could eat yogurt and cream of wheat, ice cream, and creamy soups and he was excited. Slowly some of the IV’s started coming out. Scott started eating more. He was ready to come home. 18 days after we came to the hospital for what we hoped would be laproscopic surgery, we were going home. I was beyond happy to have him home with me again, but for me the scariest part was just starting. I was now going to be the full time caregiver.
It's been a little more than a month since Scott’s surgery. There’s a six to eight week recovery period. That means no driving, no picking up anything over five pounds, no excessive bending, so that leaves the housework to me. There have been so many doctor’s appointments, so many prescriptions to pick up, four dogs to corral, plus my own life and responsibilities. I was thrust into this job of caregiver again. Each day brought new hurdles, from the mundane to the terrifying. I was drained, sleep-deprived, and at times emotionally shattered. Yet, there were moments—a shared smile, a look of gratitude from Scott—that reminded me why I kept going.
There are so many lessons I learned from this experience of being a caregiver, sometimes I joke I should write a book. Through all of this, I've realized that caregiving isn't about having the natural instincts of a nurse or the patience of a saint. It’s about showing up when you’re needed, even when you’re scared, exhausted, or unsure of what to do next. It’s about loving someone so fiercely that you’re willing to face any challenge by their side, even if it drains you in ways you never anticipated.
I've learned that caregiving is messy, complicated, and emotionally overwhelming—but it’s also a privilege. I may not have chosen this role, but stepping into it has taught me strength, resilience, and a kind of love that I didn’t know I was capable of. As I move forward, I know that while life may continue to throw challenges my way, I’ve already survived so much. And maybe, someday, I really will write that book. But for now, I'm just grateful for the days I have with Scott, for the little victories we celebrate, and for the courage I’ve found within myself, one day at a time.