In November 2017, just two months after an "all-clear" mammogram, Leslie Ferris Yerger was diagnosed with stage 4 breast cancer. The shocking news spurred her to investigate how the density of her breasts may have contributed to her cancer being overlooked.
“I realized that having breast cancer missed on mammograms was a systemic problem. I knew that I could not keep this a secret. I had to let people know. I didn’t want my story to become their story. I realized that if nothing changed, there would be more stories like mine,” Yerger explained.
Now, change has arrived. As of September 10, 2024, the U.S. Food and Drug Administration (FDA) implemented a new requirement under the Mammography Quality Standards Act (MQSA). The rule mandates that all mammogram facilities notify patients about their breast density after screenings. This major step is part of the FDA's broader efforts to improve breast cancer detection and provide women with critical information to make informed decisions about their health.
What Does This Mean for Patients?
Dr. Chrisette Dharma of Southwest Family Medicine explains that under this new rule, mammogram results will indicate whether a patient has breast tissue categorized as A or B—both indicating more fatty tissue where abnormalities are easier to detect. Alternatively, results may classify a patient’s breasts as C or D, meaning their breasts are denser, which could make it more difficult to identify potential cancers through mammograms alone.
“Patients with dense breasts might need further imaging to ensure nothing is missed,” Dr. Dharma noted. These additional tests could include ultrasounds or MRIs, which are better suited to detect abnormalities in dense breast tissue.
Understanding Breast Density
Breast density refers to the proportion of fibrous and glandular tissue versus fatty tissue in a woman’s breasts. Women with dense breasts have more glandular and fibrous tissue, which appears white on a mammogram—just like cancerous tumors—making it more difficult to detect abnormalities. An estimated 40-50% of women over the age of 40 have dense breasts, which not only increases the challenge of cancer detection but also slightly elevates the risk of developing breast cancer.
For many years, women were often unaware of their breast density, which left them uninformed about how it might affect the accuracy of their mammograms. The new FDA ruling changes that by ensuring that every woman receives this critical information.
“The National Consortium of Breast Centers (NCBC) supports the FDA’s new ruling emphasizing the importance of breast density in cancer detection. Educating and empowering patients to understand their own bodies plays a vital role in early detection.
While mammograms remain the first line of defense against breast cancer, they are not the only method of detection. For individuals with dense breast tissue, compression during a mammogram helps improve visibility. However, if the tissue cannot be adequately examined due to density, additional imaging techniques such as ultrasound or MRI should be used as needed. Combining these imaging modalities offers the comprehensive information necessary for a complete and accurate assessment,” stated Kimberly Samuels, CEO of NCBC.
NCBC has a mission to improve breast care for patients and care providers through a variety of programs and initiatives.
The Four Categories of Breast Density
Mammogram results under the new rule will categorize breast tissue into one of four groups:
· A: Almost entirely fatty
· B: Scattered areas of fibroglandular density
· C: Heterogeneously dense
· D: Extremely dense
Women with heterogeneously dense or extremely dense breasts (categories C and D) may be advised to undergo supplemental screenings such as breast ultrasound or MRI. These additional imaging methods can provide a clearer view of the breast tissue, improving the chances of detecting cancer early.
My Density Matters: Advocacy for Awareness
Yerger didn’t stop with her own diagnosis—she turned it into action. She founded My Density Matters, an organization dedicated to spreading awareness about breast density and encouraging women to take control of their breast cancer screening.
“I created My Density Matters three and a half years ago to empower women to go beyond the mammogram,” Yerger said. “I wanted to ensure that they did additional screening if necessary because of their dense breasts. I wanted to make sure that they could find their cancer early while it’s still curable and more treatable.”
Improving Communication and Early Detection
The primary goal of the new FDA rule is to enhance communication between patients and healthcare providers, allowing for more personalized breast cancer screening plans. By ensuring that women are informed about their breast density, the rule empowers patients to take proactive steps, particularly those who need more than just a standard mammogram for effective cancer detection.
Breast cancer remains one of the most common cancers among women, and early detection is key to improving survival rates. The breast density notification requirement is part of a larger effort to promote early detection, making it easier for patients and healthcare professionals to consider additional screening methods when necessary.
What Happens Next?
For women who receive mammograms after September 10, 2024, breast density information will be a routine part of their results. If a woman is found to have dense breasts, it’s crucial that she discusses the potential implications with her healthcare provider. Based on her risk factors, family history, and personal preferences, additional screenings may be recommended.
Yerger hopes this ruling will spark meaningful conversations between patients and doctors. “We want people to read their report, understand their density, and talk to their doctor,” she said. “We need to have those conversations. Imagine if everybody just did that.”
The Path Forward
The FDA’s new breast density notification rule marks a significant shift in breast cancer screening. By making breast density information available to all patients, women are better equipped to navigate their health options and take action if further testing is needed.
For Yerger, and countless others affected by dense breast tissue, the new ruling is a victory in the fight for better breast cancer detection. It opens the door for women to be more informed and proactive in safeguarding their health, ensuring that fewer cancers are missed, and more lives are saved.
“NCBC applauds Yerger’s efforts with My Density Matters for not stopping at her diagnosis and helping create a clear path forward that empowers women to understand their breast density through their mammogram report,” said Samuels.













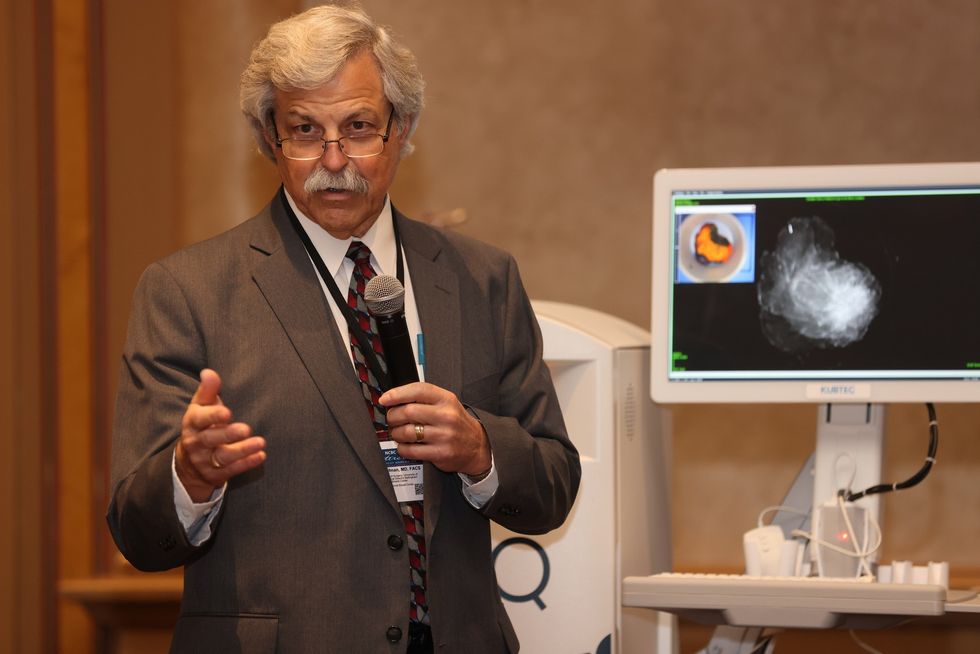 Dr. Cary S. Kaufman teaches the "Essentials of Oncoplastic Surgery" course through the National Consortium of Breast Centers, providing breast surgeons around the world with advanced techniques for optimal breast surgery outcomes.
Dr. Cary S. Kaufman teaches the "Essentials of Oncoplastic Surgery" course through the National Consortium of Breast Centers, providing breast surgeons around the world with advanced techniques for optimal breast surgery outcomes.

