Health concerns in the Asian community are multifaceted and influenced by genetic, environmental, cultural, and socio-economic factors. Understanding these health issues is crucial for providing effective healthcare and improving overall well-being in this diverse population. Here, we explore some prevalent health concerns within the Asian community and the importance of addressing them.
1. Cardiovascular Diseases
Cardiovascular diseases (CVD) are a significant health concern among Asians. Research shows that South Asians, in particular, have a higher predisposition to heart diseases compared to other ethnic groups. According to the American Heart Association, South Asians are more likely to experience coronary artery disease at a younger age and with greater severity. This heightened risk is often attributed to a combination of genetic factors, dietary habits, and a higher prevalence of conditions such as diabetes and hypertension .
2. Diabetes
Diabetes is another major health issue affecting the Asian community. Studies indicate that Asians are at a higher risk of developing type 2 diabetes compared to Caucasians, even at lower body mass indexes (BMIs). A study published in the Diabetes Care journal highlights that Asian Americans are more likely to develop diabetes at a younger age and with a lower BMI, underscoring the need for early screening and intervention in this population .
3. Hepatitis B
Hepatitis B is a significant health concern, particularly among East Asian and Southeast Asian populations. The Centers for Disease Control and Prevention (CDC) reports that Asians are disproportionately affected by chronic Hepatitis B, with an estimated 1 in 12 Asian Americans living with the virus. Chronic Hepatitis B can lead to severe liver diseases, including cirrhosis and liver cancer, making early detection and vaccination critical .
4. Cancer
Certain types of cancer have a higher incidence in the Asian community. For instance, liver cancer rates are significantly higher among Asians, largely due to the prevalence of chronic Hepatitis B. Additionally, nasopharyngeal carcinoma, a type of throat cancer, is more common in Southeast Asians. The National Cancer Institute notes that genetic factors, environmental exposures, and infectious agents contribute to these elevated cancer risks in Asian populations .
5. Mental Health
Mental health is an often-overlooked aspect of health in the Asian community. Cultural stigma surrounding mental health issues can lead to underreporting and inadequate treatment. According to the Asian American Psychological Association, Asian Americans are less likely to seek mental health services compared to other ethnic groups. Barriers include language difficulties, lack of culturally competent care, and stigma associated with mental illness .
6. Osteoporosis
Osteoporosis is another health concern prevalent among Asian populations, particularly women. Despite having lower overall body weights, Asian women are at a higher risk for osteoporosis and related fractures. Research published in the Osteoporosis International journal indicates that lower bone mineral density, dietary factors, and genetic predisposition contribute to this increased risk .
Addressing health concerns in the Asian community requires a multifaceted approach that includes awareness, early screening, culturally competent healthcare, and targeted interventions. By recognizing and understanding these specific health risks, healthcare providers can better serve the Asian population, improving health outcomes and quality of life.
References
- American Heart Association. (2019). Cardiovascular disease and risk factors in South Asians. Retrieved from Heart.org.
- Diabetes Care. (2018). Type 2 diabetes among Asian Americans. Retrieved from Diabetesjournals.org.
- Centers for Disease Control and Prevention. (2020). Hepatitis B among Asian Americans. Retrieved from CDC.gov.
- National Cancer Institute. (2019). Cancer health disparities. Retrieved from Cancer.gov.
- Asian American Psychological Association. (2017). Mental health in the Asian community. Retrieved from AAPAonline.org.
- Osteoporosis International. (2020). Osteoporosis in Asian populations. Retrieved from Springer.com.









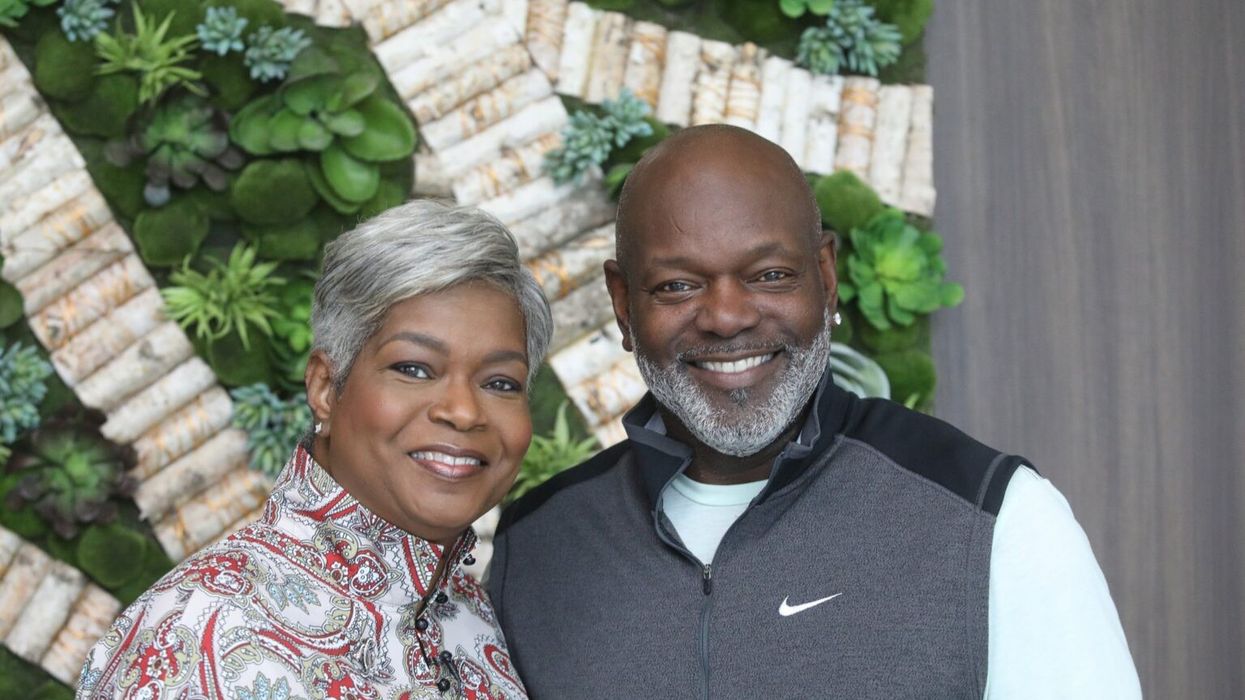
 Karla Mingo believes that her greatest gift as a cancer survivor is the ability to live with gratitude and thankfulness.
Karla Mingo believes that her greatest gift as a cancer survivor is the ability to live with gratitude and thankfulness.



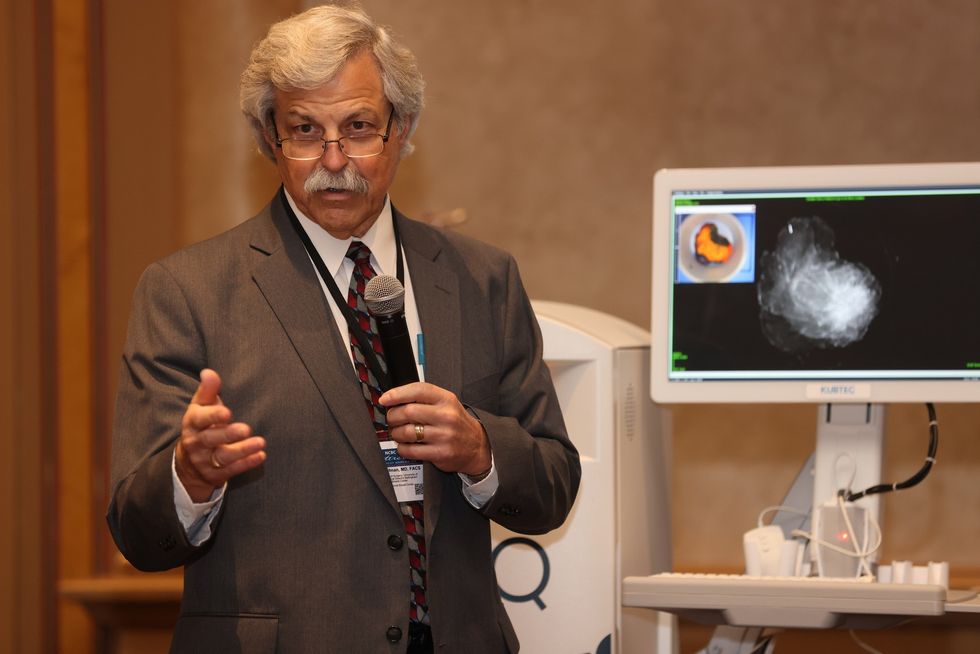 Dr. Cary S. Kaufman teaches the "Essentials of Oncoplastic Surgery" course through the National Consortium of Breast Centers, providing breast surgeons around the world with advanced techniques for optimal breast surgery outcomes.
Dr. Cary S. Kaufman teaches the "Essentials of Oncoplastic Surgery" course through the National Consortium of Breast Centers, providing breast surgeons around the world with advanced techniques for optimal breast surgery outcomes.